Mechanics of Ventilation
- Mechanics of Ventilation
- Basics of Mechanical Ventilation
- Phase Variables
- Common Modes of Ventilation
- Volume Assist-Control Ventilation (VC/AC or VCV)
- Pressure Assist-Control Ventilation (PC/AC or PCV)
- Pressure Support Ventilation (PSV)
- Synchronized Intermittent Mandatory Ventilation (SIMV)
- Pressure-Regulated Volume Control (PRVC)
- Airway Pressure Release Ventilation (APRV)
- Neurally-Adjusted Ventilatory Assist (NAVA)
- Dyssynchrony
- Disease Specific Ventilation
- Complications of Mechanical Ventilation
- Liberation from Mechanical Ventilation
- Non-Invasive Ventilation
Basics of Mechanical Ventilation
- Spontaneous breathing is considered to be negative pressure ventilation where the movement of air is a result of work done by patient's respiratory muscles
- Positive pressure ventilation is a result of movement of air from applying positive pressure to the airway (through ETT, tracheostomy, Noninvasive Mask)
- Recall the mechanics of spontaneous breathing
- Inspiratory Cycle for Spontaneous Breathing
- Diaphragm and Other Inspiratory Muscles contract -> abdominal contents pushed downward & rib cage upward and outward
- Increase intrathoracic volume (volume of the intrapleural space)
- ∴ Decrease intrapleural pressure (recall Boyle’s Law)
- ∴ Increase transpulmonary pressure (recall PTP = PALV – PPL ) -> lungs will inflate (i.e. increase in volume — again Boyle’s Law)
- ∴ Increase in lung volume -> Decrease in PALV (again Boyle’s Law)
- Making PALV lower than PATM ∴ air flows into the lungs until PALV = PATM
- Expiratory Cycle for Spontaneous Breathing
- When quiet – Passive!
- i.e. no active contraction of respiratory muscles is required for expiration to occur
- everything relaxes to its previous position
- Causing chest wall to recoil
- ∴ Decrease in intrathoracic volume
- ∴ Increase in intrathoracic pressure i.e. intrapleural perssure
- ∴ Decrease in PTP (recall PTP = PALV – PPL)
- ∴ Lungs will deflate -> Decrease in lung volume
- ∴ Increase in PALV
- Making PALV higher than PATM ∴ air flows out of the lungs until PALV = PATM
- When quiet – Passive!
- Inspiratory Cycle for Spontaneous Breathing
- Inspiratory Cycle for Positive Pressure Ventilation
- Ventilator increases airway opening pressure/PAW/PAO
- Air flows into lungs
- Increase in alveolar pressure
- Increase in transpulmonary pressure
- Increase in lung volume
Phase Variables
- Breathing is repeated cycles of inspiration and expiration
- Each breath = one cycle of inspiration followed by expiration which can be broken down into four components or phase variables
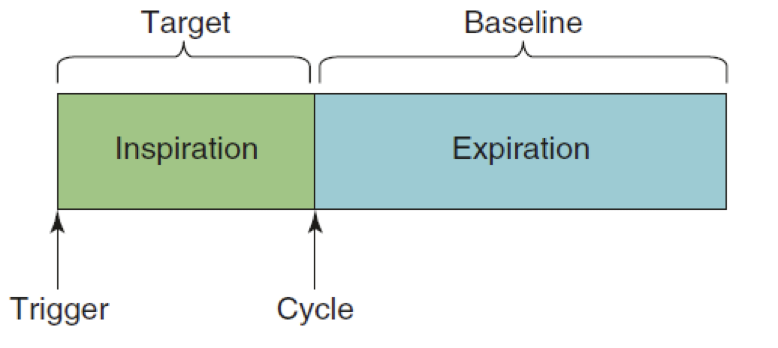
- Trigger variable -- how inspiration begins
- Target variable -- how flow is delivered during inspiration
- Cycle variable -- how inspiration ends
- Baseline variable -- proximal airway pressure during expiration
Trigger Variable
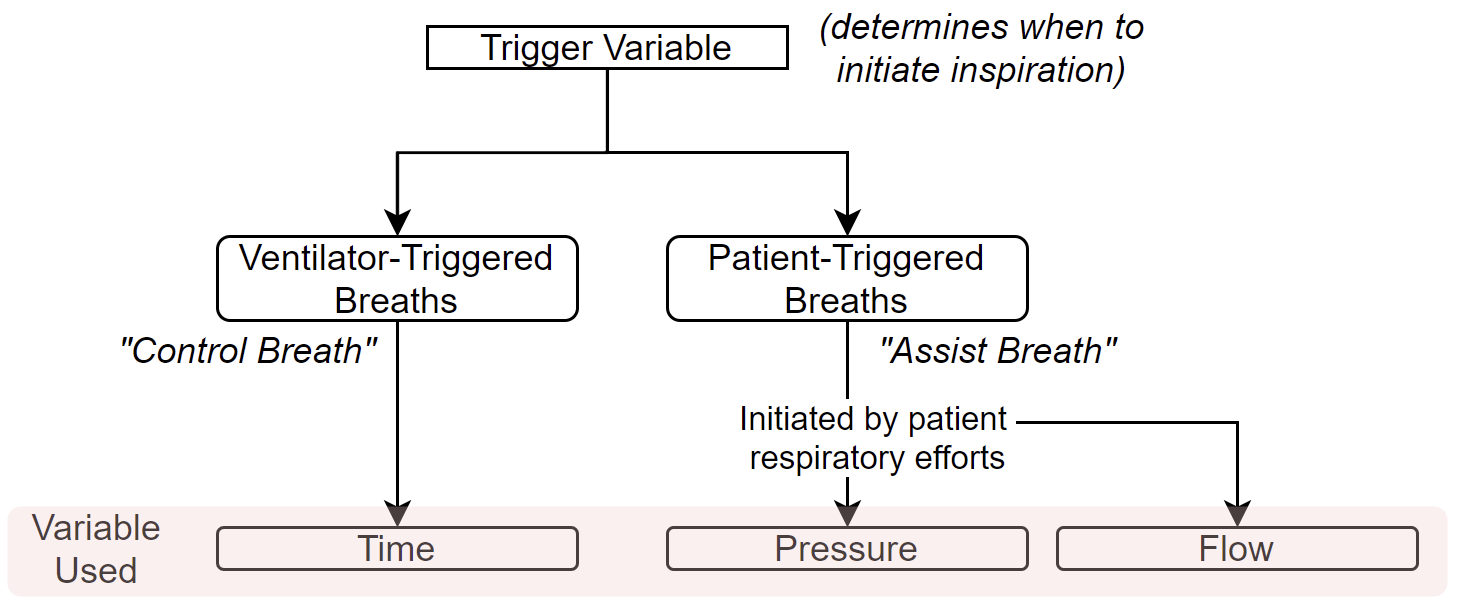
- Ventilator-Triggered Breaths
- Called "Controlled Breaths"
- Time Triggered
- Ventilator initiates a breath after a certain time
- Most common way to set this time is with
- Respiratory rate (RR)
- Time = 1/RR
- RR = 12 breaths/min
- Time = 1/12 breaths/min = 5 seconds/breath
- This means 1 breath every 5 seconds (both inspiration and expiration)
- Short way -> 60 seconds/ RR (breaths/min)
- Patient-Triggered Breaths
- Called "Assisted Breaths"
- Changes in pressure or flow in the circuit (due to patient's respiratory efforts) get detected by the ventilator
- NOTE: A patient can only trigger a breath for the next breath during the previous breath's expiratory baseline variable
- If a patient attempts to trigger a breath (i.e. has respiratory efforts) during an active inspiration (e.g. ventilator is giving a breath (controlled breath)), it will NOT trigger another breath
- the ventilator will not allow the patient to trigger a breath during an active inspiration
- If a patient attempts to trigger a breath (i.e. has respiratory efforts) during an active inspiration (e.g. ventilator is giving a breath (controlled breath)), it will NOT trigger another breath
- NOTE: A patient can only trigger a breath for the next breath during the previous breath's expiratory baseline variable
- Pressure Triggered
- Recall: inspiratory muscles contract -> decrease intrapleural pressure → decreases proximal airway pressure
- If pressure trigger is set as our trigger variable → the reduced proximal airway pressure is transmitted along the ventilator tubing and recognizing by the ventilator
- If the change in proximal airway pressure (the amount that it decreases) is greater than the set pressure trigger threshold, then a breath is initiated and delivered by the ventilator.
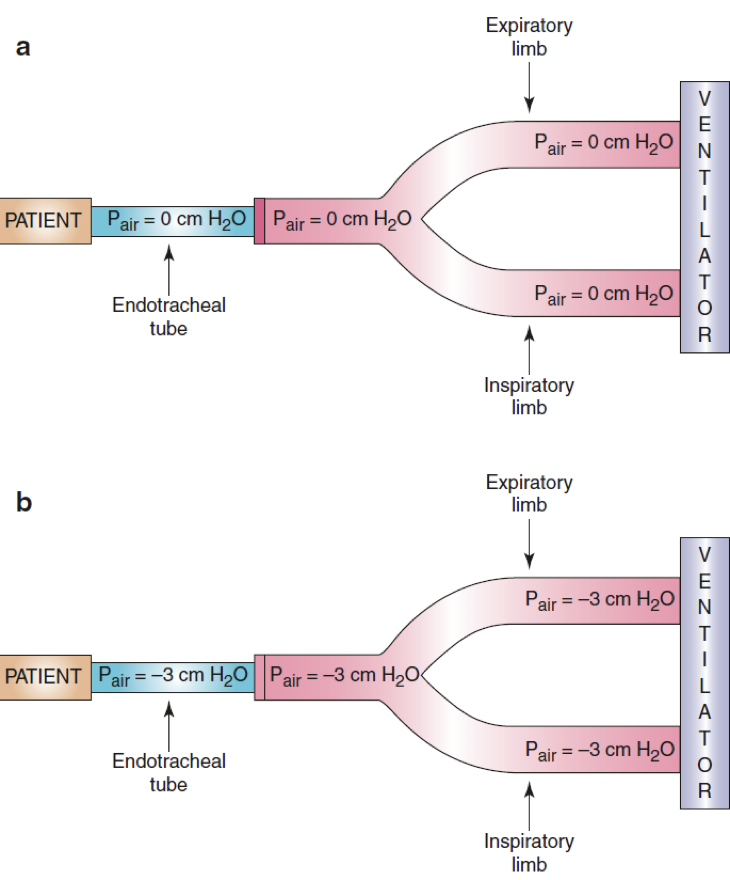
- In this example, the pressure trigger was set to recognize a drop of >2 cm H₂O and the pressure change or difference is 3 cm H₂O (i.e. it dropped by 3), which is more than the threshold therefore the ventilator will initiate a breath delivery
- Flow Triggered
- In equilibrium a continuous amount of gas flows from inspiratory limb of ventilator to expiratory limb of ventilator (e.g. 10 L/min)
- When a patient has an inspiratory effort → some of that gas flow goes to the patient (e.g. 3 L/min) and less is returned to the expiratory limb (e.g. 7 L/min)
- If flow is set as our trigger variable → the ventilator recognizes the change of flow → meets decrease in flow threshold → breath initiated by the ventilator
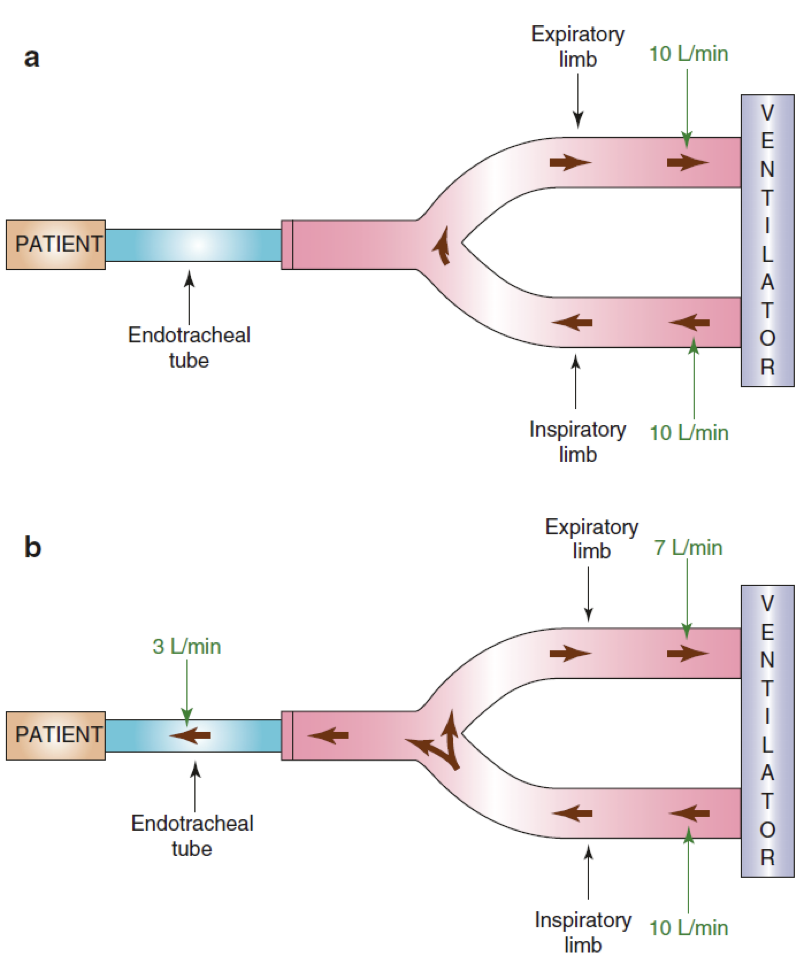
- In this example, the flow trigger is set to recognize a drop in flow of 2 L/min. The patient took 3 L/min of the flow so this is a higher drop in flow than the set threshold → breath initiated by the ventilator
- Hybrid Trigger Mode: Assist/Control
- Both RR (i.e. time trigger/ventilator-triggered/Control) and either pressure or flow trigger (i.e. patient-triggered/Assist) are SET
- If an amount of time (based on 60/RR) has elapsed without a patient-triggered breath, the ventilator will initiate a breath ("Controlled Breath")
- If the patient triggers the ventilator prior to the timed breath, the ventilator will recognize the patient's attempt and assist the breath and the time trigger clock resets
- A/C only refers to the trigger variable, not to the other phase variables
Target Variable
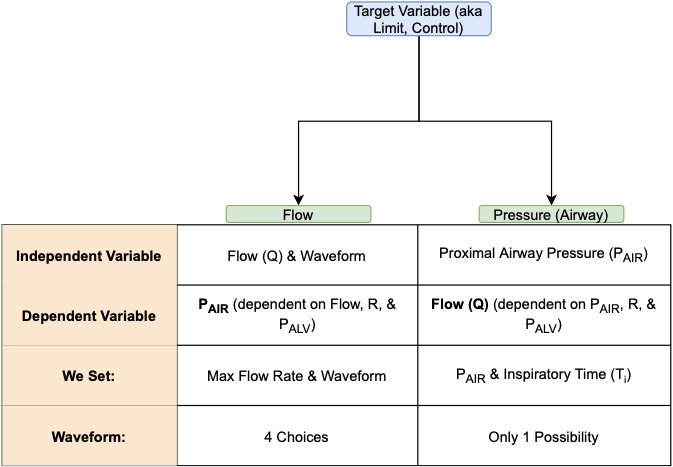
- Two options: Flow & Pressure (Airway Opening Pressure or Proximal Airway Pressure)
- Most misunderstood
- multiple names: "control" and "limit"
- This variable regulates HOW A BREATH is delivered during inspiration
- Volume does not tell us how a breath is delivered
- FLOW (which is Volume/Time) tells us how it is delivered
- Delivered over a short period of time (high flow rate)
- Delivered over a long period of time (low flow rate)
- Role of the target variable
- \(Flow\ (Q) = \left(\frac{(Airway\ Opening\ Pressure\ -Alveolar\ Pressure)}{Airway\ Resistance}\right)\)
- The set target variable will be the independent variable -- either Flow or Proximal Airway Pressure (Airway Opening Pressure)
- The other will automatically become the dependent variable
- If flow is the set target variable => independent variable: the proximal airway pressure, airway resistance and alveolar pressure => dependent variables (i.e. they depend on the flow)
- If proximal airway pressure is the set target variable => independent variable: the flow, airway resistance and alveolar pressure => dependent variables (i.e. they depend on the proximal airway pressure)
- The other will automatically become the dependent variable
- Flow Targeted
- Ventilator will deliver the flow set by the provider i.e. independent variable
- Dependent variables = the proximal airway pressure, airway resistance and alveolar pressure
- Provider also sets the flow waveform pattern which describes the pattern of gas flow
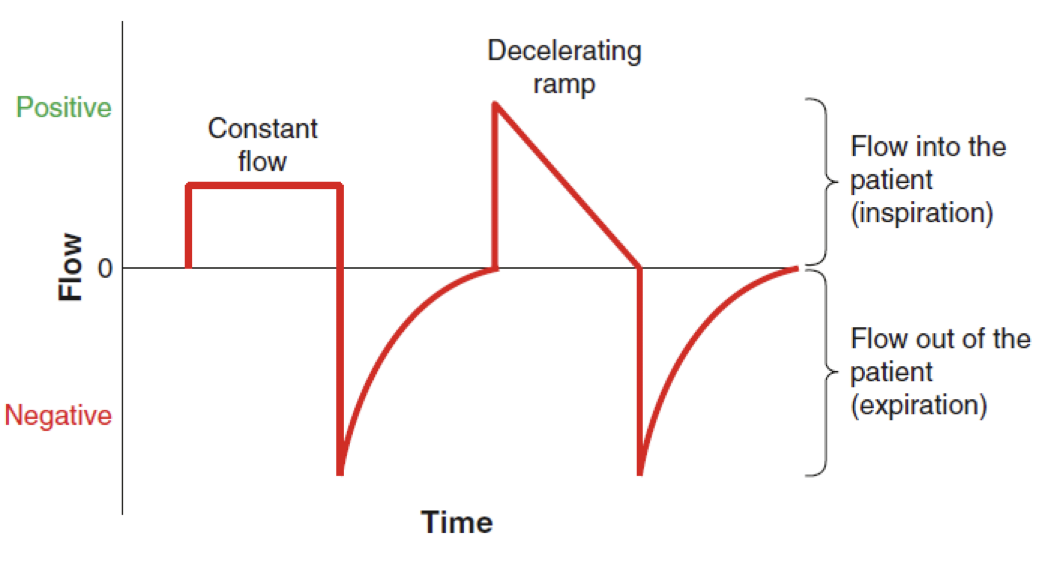
- Constant flow -- square waveform or rectangle waveform -- inspiratory flow rate instantly rises to the set level and remains constant during the inspiratory cycle
- Decelerating ramp -- inspiratory flow rate is highest at the beginning of inspiration, when patient's flow demand is greatest and then depreciates to zero flow
- Usually happens in pressure control or pressure support ventilation where the proximal airway pressure is constant i.e. the independent variable
- So alveolar pressure increases and the flow at which this happens is highest at the beginning of the breath and then tapers off as alveolar pressure continues to increase
- Usually happens in pressure control or pressure support ventilation where the proximal airway pressure is constant i.e. the independent variable
- Ventilator will deliver the flow set by the provider i.e. independent variable
- Pressure Targeted
- Ventilator will deliver the flow to quickly achieve and maintain proximal airway pressure that is set by the provider during inspiration making it the independent variable
- Dependent variables = flow, airway resistance and alveolar pressure
- Waveform will automatically be produced → decelerating ramp flow
- Recall \(Flow\ (Q) = \left(\frac{(Airway\ Opening\ Pressure\ -Alveolar\ Pressure)}{Airway\ Resistance}\right)\)
- During inspiration, air fills alveoli → increase in alveolar pressure, but since the provider set the proximal airway pressure (i.e. constant) and the resistance of the system remains unchanged; to adjust for the increase in alveolar pressure, the flow has to decrease → flow will be highest at the beginning of the breath when the alveolar pressure is the lowest and flow will decrease as the inspiratory phase proceeds => decelerating ramp
- Ventilator will deliver the flow to quickly achieve and maintain proximal airway pressure that is set by the provider during inspiration making it the independent variable
- How to differentiate between flow targeted & pressure targeted ventilation
- When a change in the respiratory system occurs by either (1) change in resistance or compliance or (2) change in patient's respiratory efforts
- Recall the set target variable will remain unchanged, so the dependent variable changes because flow and pressure cannot change simultaneously.
- Change in Respiratory System: Increased Resistance (e.g. biting of ETT)
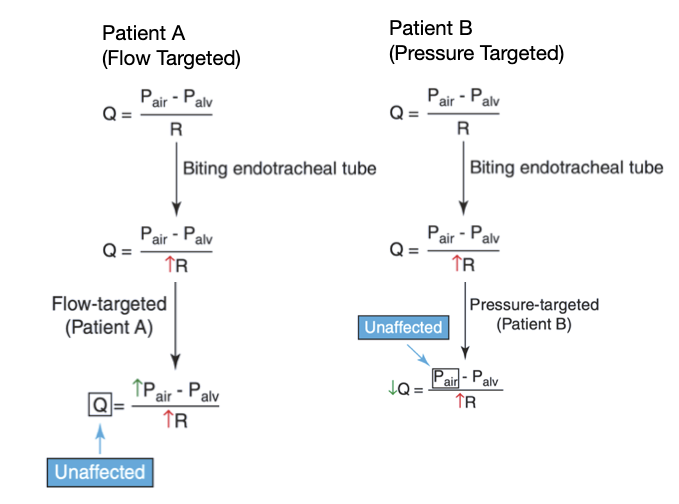
- In a patient on a flow targeted mode of ventilation, and increase in resistance with unaffected flow (due to it being set by the provider), will have to cause an increase in proximal airway pressure (to make sure flow stays unaffected)
- In a patient on a pressure targeted mode of ventilation, and increase in resistance with unaffected pressure (due to it being set by the provider), will have to cause a decrease in the flow
- Change in Patient's Respiratory Effort: Increased effort → Decrease in alveolar pressure
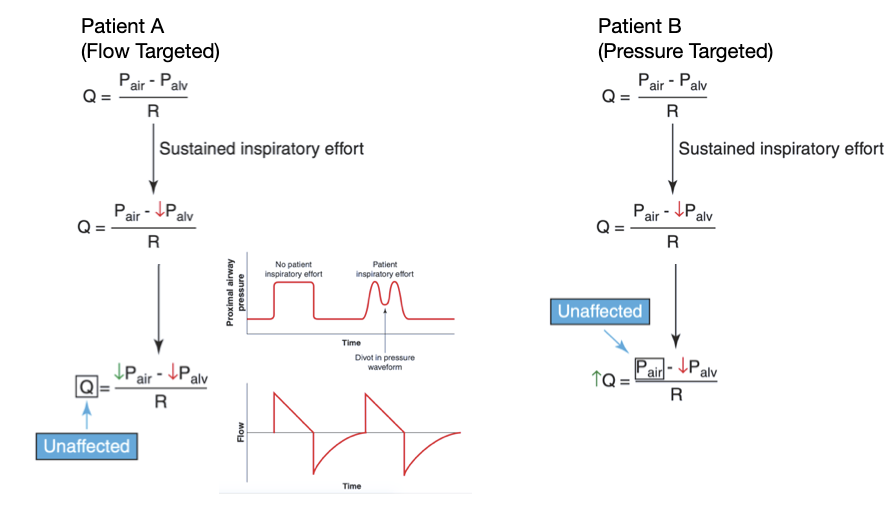
- In a patient on a flow targeted mode of ventilation, and increased patient effort (i.e. decrease in alveolar pressure) with unaffected flow (again set by the provider), the proximal airway pressure will have to decrease to make sure flow is unaffected
- In a patient on a pressure targeted mode of ventilation, and increased patient effort (i.e. decrease in alveolar pressure) with unaffected proximal airway pressure (again set by the provider), the flow will have to increase to make sure proximal airway pressure is unaffected
- When a change in the respiratory system occurs by either (1) change in resistance or compliance or (2) change in patient's respiratory efforts
Cycle Variable
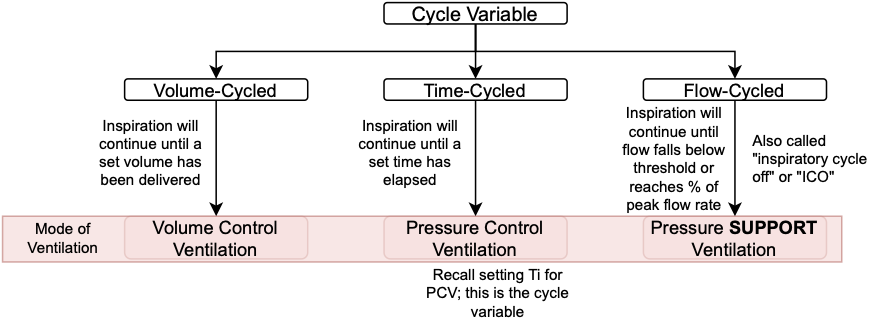
- How inspiration ends; you have to tell the ventilator to stop delivering a breath
- Three options: Volume, Flow, Time
- Volume Cycled
- Inspiration will continue until a set volume has been delivered
- Once that volume has been delivered → inspiration will stop (i.e. will cycle off)
- Flow Cycled
- Inspiration will continue until the flow rate falls below a set threshold (i.e. it reaches a certain % of the peak flow rate -- ICO, inspiratory cycle off)
- Once the flow rate goes below that threshold (or hits that %) → inspiration will stop (i.e. will cycle off)
- e.g. if ICO is set to 20%, then ventilator will terminate a breath once the flow drops below 20% of the peak flow rate
- What would happen to the duration of the breath if ICO is unchanged from 20% to 30%
- Duration of inspiration will be shorter since 30% will be reached before 20% would
- How do you manipulate time in pressure support ventilation?
- Manipulate the ICO (i.e. flow cycle)
- Increase ICO → shorter duration of inspiration
- Decrease ICO → longer duration of inspiration
- Manipulate the ICO (i.e. flow cycle)
- Time Cycled
- Inspiration will continue until a certain time has elapsed
- Once that time has elapsed → inspiration will stop (i.e. will cycle off)
- No pressure cycle because pressure cycle is usually a back up safety measure to prevent high pressures
Baseline Variable
- Refers to the proximal airway pressure during expiration
- If this pressure is equal to atmospheric pressure it is referred to has zero end-expiratory pressure (ZEEP)
- Ventilator allows for complete recoil of lung and chest wall; we usually do not set this equal to atmospheric pressure
- if this pressure is above the atmospheric pressure it is referred to has positive end-expiratory pressure (PEEP)
- Therefore: baseline variable = PEEP
Common Modes of Ventilation
Volume Assist-Control Ventilation (VC/AC or VCV)
- Trigger variable: Flow/Pressure and/or Time (Both if its AC)
- Target variable: Flow targeted -- we set: max flow rate, waveform and tidal volume; since we set the flow and the volume, inspiratory time is automatically set (F = V/T), this inspiratory time is a portion of the total time set by the trigger variable (which includes both inspiration and expiration)
- Therefore in VC/AC, inspiratory time cannot be altered by patient respiratory effort or by changes in the respiratory system
- Total time can still be altered by patient respiratory effort (increase in RR means shorter total time of breath) but the inspiratory time remains constant
- Patient initially breathes 10 breaths per min, that is 1 breath every 6 seconds (60/10) and if we set the flow at 60 L/min (which is 1 L/second) and the tidal volume is set to 500 mL (0.5 L), the Ti would be automatically set to 0.5 seconds (0.5/1 L/second)
- This means of a 6 second breath, 0.5 seconds is spent on inspiration and 5.5 seconds is spent on expiration
- If the patient's RR goes up to 12 breaths per min, that is 1 breath every 5 seconds and the flow and tidal volume does not change, the inspiratory time therefore will not change.
- This means of a 5 second breath, 0.5 seconds is spent on inspiration and 4.5 seconds is spent on expiration
- Total time decreased from 6 seconds to 5 seconds but the inspiratory time did not change
- Patient initially breathes 10 breaths per min, that is 1 breath every 6 seconds (60/10) and if we set the flow at 60 L/min (which is 1 L/second) and the tidal volume is set to 500 mL (0.5 L), the Ti would be automatically set to 0.5 seconds (0.5/1 L/second)
- The way to manipulate time in VC/AC is to adjust the max flow rate -> higher max flow rate means shorter inspiratory time; lower max flow rate means longer inspiratory time
- Above example: if the patient's RR is 10 breaths per min, that is 1 breath every 6 seconds, and the flow rate is now set at 80 L/min (which is 1.33 L/second) and the tidal volume is set to 500 mL (0.5 L), the Ti would now be (0.5/1.33 L/second) which is 0.38 seconds.
- Notice the Ti went down (shorter inspiratory time) with a higher flow rate
- This means of a 6 second breath, 0.38 seconds are spent on inspiration and 5.62 seconds are spent on expiration
- This means a higher flow rate will increase the expiration time (helpful in patients with obstructive lung disease)
- Above example: if the patient's RR is 10 breaths per min, that is 1 breath every 6 seconds, and the flow rate is now set at 80 L/min (which is 1.33 L/second) and the tidal volume is set to 500 mL (0.5 L), the Ti would now be (0.5/1.33 L/second) which is 0.38 seconds.
- Total time can still be altered by patient respiratory effort (increase in RR means shorter total time of breath) but the inspiratory time remains constant
- Dependent variables: proximal airway pressure, airway resistance, alveolar pressure
- Therefore in VC/AC, inspiratory time cannot be altered by patient respiratory effort or by changes in the respiratory system
- Cycle variable: Volume
Pressure Assist-Control Ventilation (PC/AC or PCV)
- Trigger variable: Flow/Pressure and/or Time (Both if its AC)
- Target variable: Pressure targeted -- we set: proximal airway pressure and inspiratory time (Ti)
- Since we set inspiratory time, like VCV this cannot be altered by patient respiratory effort or by changes in the respiratory system
- Cycle variable: Time (the set Ti)
Pressure Support Ventilation (PSV)
- Trigger variable: Flow or Pressure (remember this mode of ventilation is patient triggered, so all breaths are assisted)
- Target variable: Pressure targeted -- we set: pressure support (how much pressure above the PEEP we want to assist the patient), inspiratory cycle off (ICO)
- Notice we do NOT set the RR since the patient will control that
- Cycle variable: Flow (the ICO)
Synchronized Intermittent Mandatory Ventilation (SIMV)
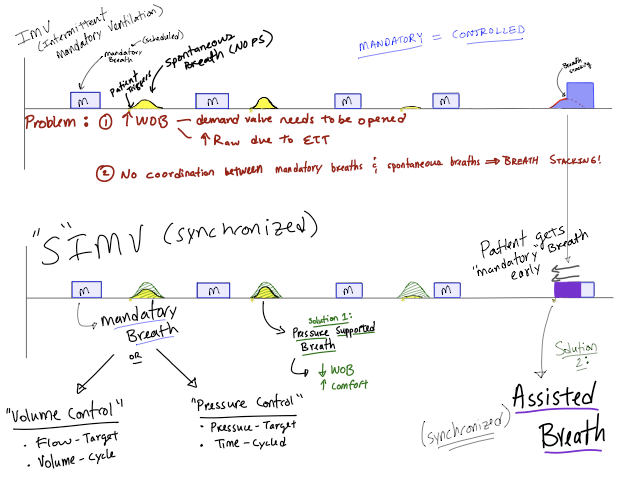
- Increases weaning failure versus PSV
- Slower at weaning than PSV or T-piece
Pressure-Regulated Volume Control (PRVC)
- Other names: volume control plus (VC+), autoflow, adaptive-pressure control, adaptive support ventilation
- Trigger variable: Flow/Pressure and/or Time (both since its assist and control)
- Target variable: Flow targeted
- In PRVC we set a goal volume to be delivered and we set an inspiratory time (F = V/T), therefore Flow is technically set and constant.
- Cycle variable: Time (set Ti)
- Differences from PCV
- Although we are setting the inspiratory time and a pressure is being delivered (similar to PCV), our target is flow where as in PCV our target is pressure because the pressure amplitude varies from breath to breath based on the previous breaths requirements to achieve a tidal volume
- Similarities to PCV
- Delivers a pressure (albeit a calculated one not a SET one)
- We set inspiratory time (Ti)
- Similarities to VCV
- Delivers a set tidal volume with the lowest possible pressure
- Called adaptive because the pressure will change over time as compliance changes
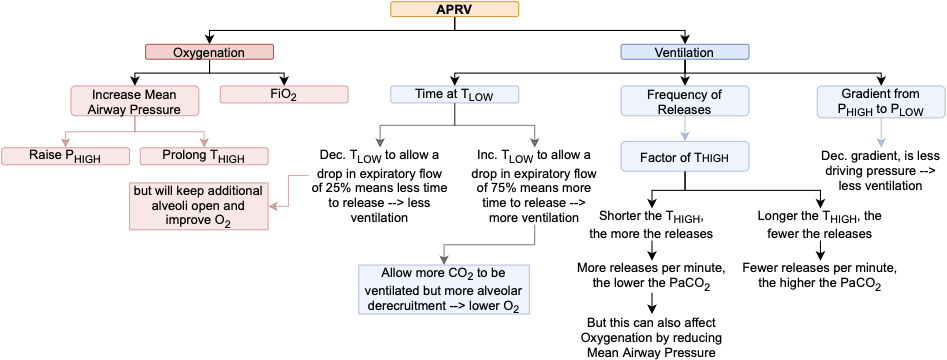
Airway Pressure Release Ventilation (APRV)
- I/E Ratio
- Refers to the amount of time spent in each phase of the respiratory cycle
- Under physiologic conditions we normally spend 2-3 times as much time in passive exhalation (I:E of 1:2 or 1:3)
- If the patient is deeply sedated or paralyzed they will breath at the RR we set
- e.g. RR = 15 breaths/min
- means a full I:E cycle is 60/15 or 4 seconds
- "I" would be 1 second and E would be 3 seconds making the I:E ratio 1:3
- Inverse I:E Ratio
- more time spent in inspiration than expiration
- very uncomfortable and can lead to breath stacking
- APRV takes the higher PEEP strategy of ARDSnet trial and takes it to a different level
- Recall severely injured lungs have a high shunt fraction (low V/Q)
- flooded or collapsed alveoli are perfused but gas cannot make it to the alveolar-capillary membrane
- Positive pressure ventilation can reduce this shunt fraction by -- recruiting, reopening and stabilizing vulnerable alveoli
- Example Patient: ARDS
- Put patient on CPAP of 35 with FiO₂ of 100%
- Oxygenation improves because CPAP would open up the alveoli and oxygen would diffuse across the alveoli into the pulmonary capillaries (increasing V/Q)
- Problem = Ventilation
- Unlikely that the patient can maintain their own minute ventilation → dramatic rise in PaCO₂ due to lack of tidal breathing
- If you give more tidal volume → attempting to push more air in on top of a CPAP of 35 => very high distending pressures even if tidal volumes were kept low
- Instead of giving more tidal volume, suddenly decompress the airways by lowering the pressure to zero
- Air will rush out → carrying CO₂ with it → adequate ventilation
- If you left the pressure at zero for too long → de-recruitment of alveoli (i.e. all vulnerable alveoli would collapse; increased risk of atelectrauma) (i.e. you would lower the V/Q again in other words increase the shunt fraction)
- Solution: Depressurize the airway long enough to let the gas escape but short enough to keep the alveoli from collapsing
- Put patient on CPAP of 35 with FiO₂ of 100%
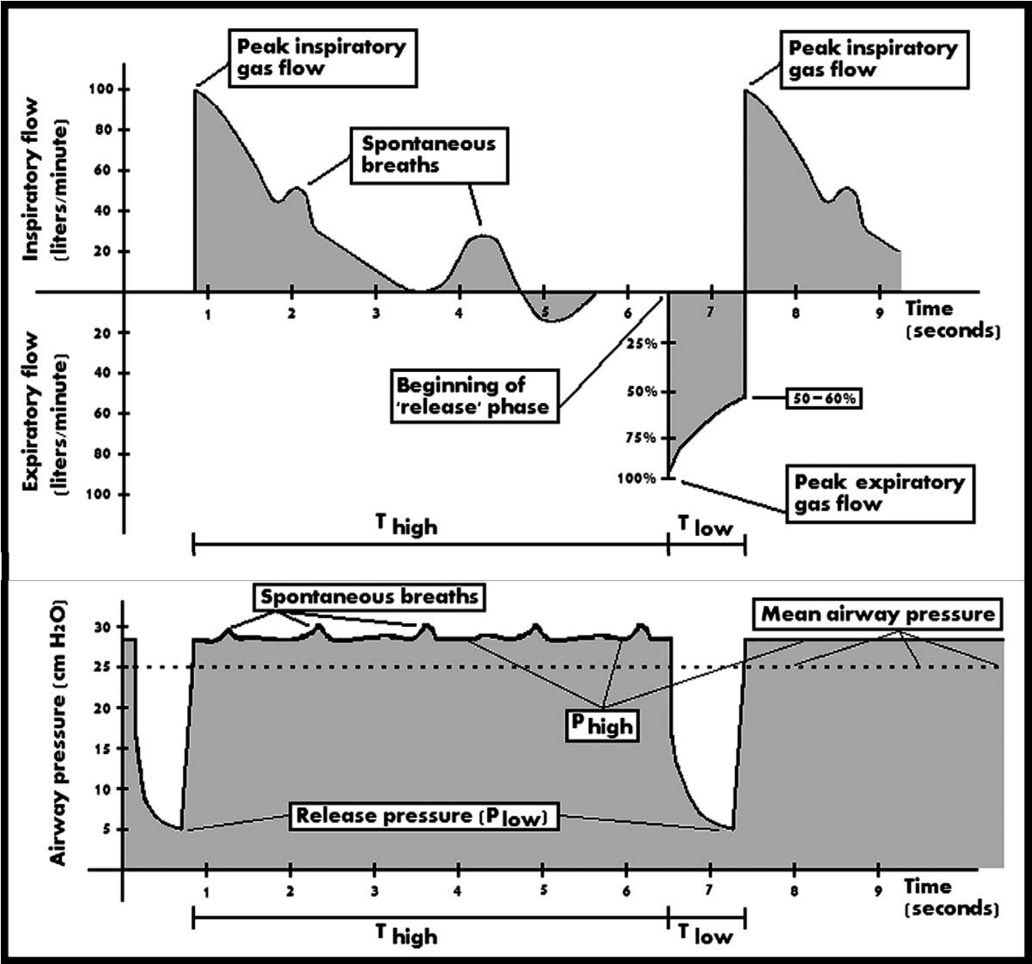
- APRV = Breathing on CPAP with intermittent releases
- CPAP there to keep lungs open and maintain oxygenation by providing adequate mean airway pressure (area under pressure time curve)
- Patient can also breath spontaneously improving V/Q matching and patient comfort while allowing some CO₂ clearance
- CPAP there to keep lungs open and maintain oxygenation by providing adequate mean airway pressure (area under pressure time curve)
- APRV Terms
- Phigh - the CPAP pressure applied to the airways during the majority of the cycle, pressure needed to maintain open alveoli
- higher Phigh means higher mean airway pressure and better oxygenation
- provides the driving pressure for the release breath
- as the patient's gas exchange and compliance improve, will need less Phigh (which is how you wean from APRV)
- Thigh - time spent at Phigh
- its the time between releases
- a longer Thigh will increase mean airway pressure and improve oxygenation but it also means fewer releases per minute (which means you will raise PaCO₂)
- Plow - pressure during releases
- generally set to 0
- airways act like a natural flow resistor, so end-expiratory pressure rarely reaches zero but having the Plow at zero creates the highest pressure gradient and facilitates better release of gas
- If you need to raise the mean airway pressure, you can increase the Plow; however, this will limit ventilation due to decreased pressure gradient
- Tlow - time spent at Plow
- usually short at 0.4 to 0.8 seconds
- this is enough time for gas to escape but short enough to keep most of the alveoli from collapsing
- If we need to ventilate more CO₂, this Tlow can be extended but this may lead to more de-recruitment
- adjust this by looking at the expiratory waveform; adjust to achieve an end-expiratory flow equal to 75% of Peak expiratory flow rate
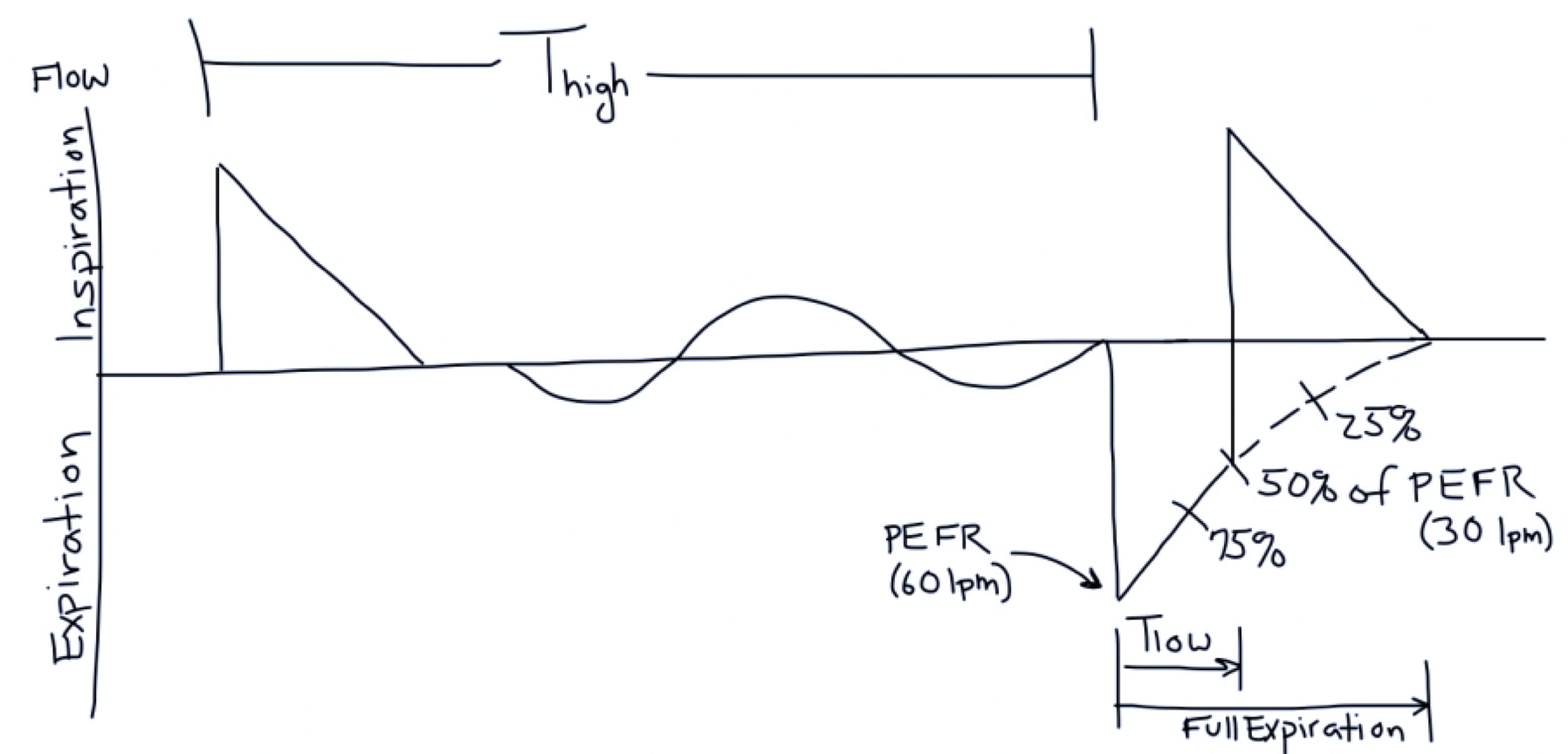
- Phigh - the CPAP pressure applied to the airways during the majority of the cycle, pressure needed to maintain open alveoli
- Compliance in APRV
- If compliance is 20 mL/cm H₂O how much gas will be released from a Phigh of 30 to a Plow of 0?
- Compliance = V/P so 20 = V/30 -> V = 600 mL
- If compliance improves then same pressure drop will have a larger release of volumes -- one way to know if patient is getting better
- Therefore compliance dictates how much gas is released
- If compliance is 20 mL/cm H₂O how much gas will be released from a Phigh of 30 to a Plow of 0?
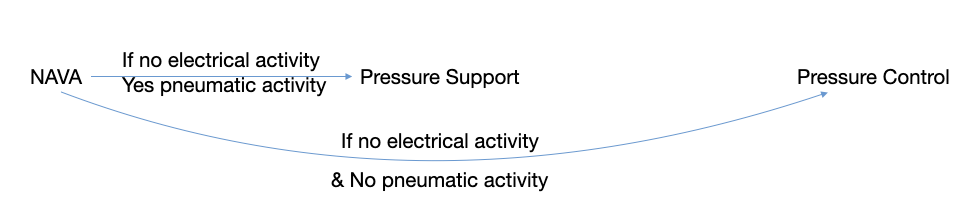
Neurally-Adjusted Ventilatory Assist (NAVA)
- adjusts pressure support based on electrical activity of the diaphragm
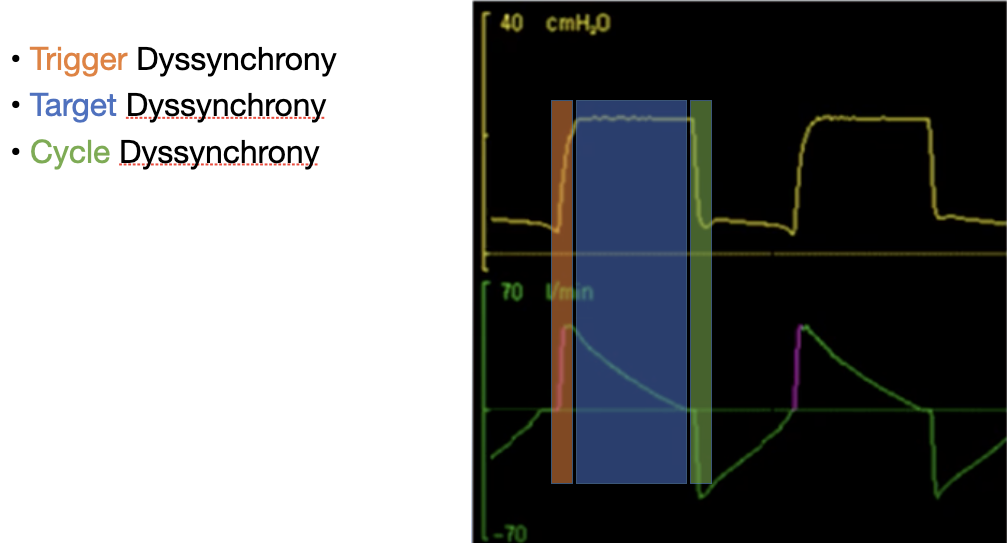
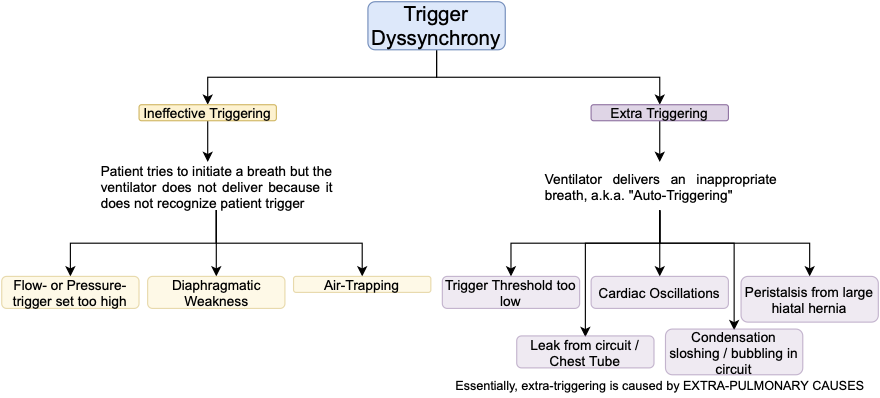
Dyssynchrony
- Any disorder in the normal or expected coordination of timed events
- Can happen in the three phase variables of inspiration and less commonly with baseline variable of exhalation